Pelvic Stress Fracture
Updated:
(Also known as Stress Fracture of the Pelvis, Pubic Ramus Stress Fracture, Pubic Bone Stress Fracture, Ischial Stress Fracture)
What is a pelvic stress fracture?
A pelvic stress fracture is a condition characterized by an incomplete crack in one of the pelvic bones.
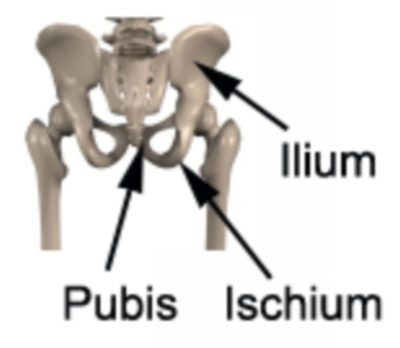
Each half of the pelvis comprises of the union of 3 bones known as the ischium, ilium and pubis (figure 1). Before puberty, these bones are separated by cartilage and eventually fuse to form one continuous bone by approximately 23 years of age. The two halves of the pelvis are called hemipelvises and together form the pelvis as a whole.
Many muscles of the hip, knee, lower back and abdomen attach to the pelvis. When these muscles contract, a pulling force is exerted on the bone. In addition, weight bearing activity places compressive forces on the pelvis via the hip joint. When these forces are excessive or too repetitive, and beyond what the bone can withstand, bony damage can gradually occur. This may initially result in a bony stress reaction, however, with continued damage may progress to a pelvic stress fracture.
The pubic ramus and ischium are two of the more commonly affected regions in a pelvic stress fracture. When these occur they are called ‘Pubic Ramus Stress Fracture’ and ‘Ischial Stress Fracture’ respectively.
Cause of a pelvic stress fracture
A pelvic stress fracture typically occurs over time with excessive weight bearing activity such as running, sprinting, jumping or dancing. They often occur following a recent increase in activity or change in training conditions (such as surface, footwear or technique changes etc) and are particularly common in long distance runners. Occasionally they may occur due to repetitive kicking in sports such as football or soccer. Pelvic stress fractures may also occur in women, following pregnancy, who commence excessive weight bearing activity without adequate pelvic and core stability.
Signs and symptoms of a pelvic stress fracture
Patients with this condition typically experience a localized pain in the pelvic region that increases with impact activity (such as running, jumping, sprinting and hopping – often causing the patient to limp) and may decrease with rest. The pain may be severe enough that it causes the patient to stop the activity.
Depending on the location of the pelvic stress fracture, pain may be felt in the buttock, groin, hip or lower back and sometimes may radiate to the thigh or knee. In severe cases, walking or standing may be enough to aggravate symptoms. Other symptoms may include night ache, pain when resting or pain on firmly touching the affected region of the bone.
Diagnosis of a pelvic stress fracture
A thorough subjective and objective examination from a physiotherapist may be sufficient to diagnose a pelvic stress fracture. Further investigations such as an X-ray, MRI, CT scan or bone scan are usually required to confirm diagnosis and determine the severity of injury.
Prognosis of a pelvic stress fracture
With appropriate physiotherapy management, most patients with a pelvic stress fracture can make a full recovery (i.e. return to sport or normal activities) in a period of 3-12 months. In more severe cases, recovery may take 1-2 years, or longer, depending on the intervention required and a range of other factors. In rare cases, some patients may experience ongoing symptoms or complications which may require further management.
Treatment for a pelvic stress fracture
Treatment for a pelvic stress fracture typically involves an initial period of rest from weight bearing activity. This may involve a period of reduced activity or the use of a walking stick or crutches for a number of weeks. Following this, a gradual increase in weight bearing activity and exercise can usually occur as tolerated, provided symptoms do not increase. This should take place over a period of weeks to months with direction from the treating physiotherapist and will vary depending on the severity of the injury and how well the contributing factors have been addressed.
Ignoring symptoms or adopting a ‘no pain, no gain’ attitude is likely to cause further damage and may slow healing or prevent healing of the pelvic stress fracture altogether. Immediate, appropriate treatment is essential to ensure a speedy recovery.
Manual “hands-on” treatment from a physiotherapist, such as massage, trigger point release techniques, dry needling, joint mobilisation, stretches, and electrotherapy, can assist with hastening healing, improving range of movement, pain and function and correcting factors that have contributed to the development of the pelvic stress fracture. This can generally commence once the physiotherapist has indicated it is safe to do so.
Patients should also perform specific pain free flexibility and strengthening exercises as part of their rehabilitation to ensure an optimal outcome. Particular emphasis is placed on improving pelvic stability and core stability. Alternative activities which place minimal weight bearing forces through the affected bone should be performed to maintain fitness (such as swimming, cycling and water running). The treating physiotherapist can advise which exercises and activities are most appropriate for the patient and when they should be commenced.
In the final stages of rehabilitation for a pelvic stress fracture, a gradual return to activity or sport can occur as guided by the treating physiotherapist, provided symptoms do not increase. This may involve a gradual return to running program to recondition the pelvis to running in a safe and effective manner.
Appropriate footwear advice and / or the use of orthotics may also be indicated in those patients whose lower limb biomechanics are likely to have contributed to the development of the pelvic stress fracture. Running technique, as well as training technique or training methods, may also need addressing to decrease the likelihood of injury recurrence.
Contributing factors to the development of a pelvic stress fracture
There are several factors which may contribute to the development of a pelvic stress fracture. These need to be assessed and, where possible, corrected with direction from the treating physiotherapist. Some of these factors include:
- muscle weakness (particularly of the gluteals, pelvic stabilisers and core stabilisers)
- pelvic instability (often following pregnancy)
- poor flexibility (particularly of the gluteals, hip flexors, abdominals, adductors, hamstrings or quadriceps)
- joint stiffness (particularly of the hip, lumbar spine, knee or ankle)
- poor balance
- inappropriate footwear
- poor foot posture (especially flat feet or high arches)
- leg length discrepancies
- inappropriate or excessive training (particularly on hard or uneven surfaces)
- poor running technique
- lack of fitness or conditioning
- body weight
- age
- bone health
- inadequate diet
- menstrual disturbances (in females)
Physiotherapy for a pelvic stress fracture
Physiotherapy treatment for patients with a pelvic stress fracture is vital to hasten healing, prevent injury recurrence and ensure an optimal outcome. Treatment may comprise:
- soft tissue massage
- joint mobilization
- joint manipulation
- exercises to improve strength, fitness, balance, flexibility and core stability
- Clinical Pilates
- electrotherapy
- dry needling
- the use of crutches or other walking aids
- activity modification advice
- biomechanical correction (e.g. the use of orthotics or foot taping, or, running technique correction)
- footwear advice
- education
- a gradual return to running / activity plan
Other intervention for a pelvic stress fracture
Despite appropriate physiotherapy management, some patients with this condition do not improve and require other intervention to ensure an optimal outcome. The treating physiotherapist or doctor can advise on the best course of management when this is the case. This may include further investigations such as X-rays, CT scan, MRI or bone scan, extended periods of non-weight-bearing (involving the use of crutches), review with a podiatrist (for possible orthotics) or referral to appropriate medical authorities who can advise on any intervention that may be appropriate to improve the pelvic stress fracture. Occasionally, patients with this condition may require surgery to stabilize the stress fracture and aid healing.
Exercises for a pelvic stress fracture
The following exercises are commonly prescribed to patients with a stress fracture of the pelvis. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 times daily once the physiotherapist has indicated it is safe to do so and only provided they do not cause or increase symptoms.
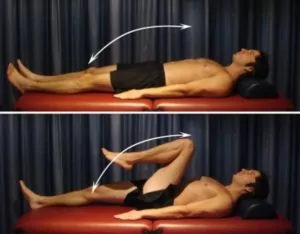
Hip & Knee Bend to Straighten
Take your knee to your chest as far as possible pain free allowing your knee to bend (figure 2). Then return to the starting position. Repeat 10 – 20 times provided there is no increase in symptoms. Then repeat on the opposite leg.
Hip External Rotation
Begin with your knee bent and foot flat on the floor. Take your knee to the side as far as possible pain-free (figure 3). Repeat 10 – 20 times provided there is no increase in symptoms. Then repeat on the other leg.

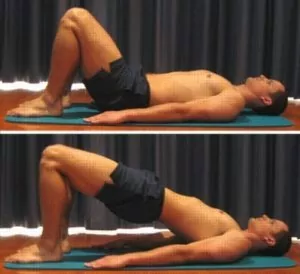
Bridging
Begin this exercise lying on your back in the position demonstrated (figure 4). Slowly lift your bottom pushing through your feet, until your knees, hips and shoulders are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds then slowly lower your bottom back down. Repeat 10 times provided the exercise is pain free.
Find a Physio
Find a Physiotherapist in your local area who can treat a pelvic stress fracture.
Physiotherapy products for a pelvic stress fracture
Some commonly recommended products by physiotherapists for patients with a pelvic stress fracture include:
To purchase physiotherapy products for a pelvic stress fracture click on one of the above links or visit the PhysioAdvisor Shop.
Other Exercises
- View more Hip Strengthening Exercises
- View more Hip Stretches
- View Lower Back Stretches
- View Leg Stretches
- View Leg Strengthening Exercises
- View Core Stability Exercises
- View Balance Exercises
More Information
- Read about Choosing a Shoe.
- Learn How to Use Crutches correctly.

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/hip-groin/pelvic-stress-fracture”>Pelvic Stress Fracture – PhysioAdvisor.com</a><br/>PhysioAdvisor offers detailed physiotherapy information on a pelvic stress fracture including: diagnosis, treatment, exercises, physiotherapy products and more...
Return to the top of Pelvic Stress Fracture.


